“What do you think?”
It was eight years ago. Dr. Julie Ann Sosa and Dr. Sanziana Roman, two leading endocrine surgeons, approached Dr. Diane Krause about growing new parathyroid cells in the lab. They wanted to treat patients — mostly women — suffering from a lack of the hormone these cells produce.
Dr. Krause, an internationally recognized stem cell researcher, was immediately intrigued.
“I thought, ‘You know what — that sounds like a good idea,’” Krause said. “But was it even feasible?”
Thanks to a pair of pilot grants from Women’s Health Research at Yale, we now know the answer is, “Yes, it is feasible.” Moreover, while the team has not yet reached their ultimate goal, they have successfully achieved critically important steps in guiding a stem cell down the path to becoming a functional parathyroid-like cell. And with new funding from WHRY this year, Krause and her collaborators continue to move closer to a cure for this condition, known as hypoparathyroidism.
“Patients contact me every week,” Krause said. “They want us to succeed. They need the breakthroughs. And that’s what keeps us going.”
What Causes Hypoparathyroidism, and What Is It?
Causes of hypoparathyroidism include autoimmune diseases and hereditary conditions that lead to depleted levels of a key hormone. But the chain of events leading toward this condition most often starts with cancer of the thyroid gland. This is an organ located in the neck that releases hormones controlling metabolic functions such as breathing, heart rate, cholesterol levels, body temperature, and more.
Women in the United States suffer from thyroid disease at rates up to eight times higher than men. Women develop thyroid cancer at a rate three times higher than men.
Krause, Professor of Laboratory Medicine, Cell Biology, and Pathology and Associate Director of the Yale Stem Cell Center, regularly hears from women who have had their thyroid glands removed to treat this cancer. To be sure that no malignant tissue remains, such surgery often involves removing the parathyroid glands, four rice-sized structures that are normally located behind the thyroid and that are responsible for maintaining the body’s calcium levels.
Without these glands and the hormone they produce, called parathyroid hormone (PTH), bones do not release this important mineral into the bloodstream when calcium levels drop. In addition, the intestines receive no signal to absorb more calcium from food, and the kidneys do not increase their ability to hold on to calcium before releasing it in urine.
Calcium deficiency can lead to serious health problems, including painful muscle spasms in the hands and feet, seizures, an irregular heartbeat, or even heart failure. Patients also suffer on a daily basis due to fatigue and “brain fog,” a less well understood aspect of the disease. Current treatments require regular calcium supplements that can be short-acting and trigger unwanted side effects, making it difficult for patients to sustain a proper balance.
A New Way Forward
Stem cells are the body’s basic, convertible building blocks. Either through natural human development or laboratory manipulations, stem cells have the potential to become any of the body’s specialized cells that serve a specific function, such as blood cells or cells that form bone or make up heart tissue.
Krause, Sosa, and Roman, also now a professor of surgery at UCSF, recruited Dr. Betty Lawton, a research associate in Krause’s lab with the technical expertise needed to complete the team. With WHRY’s grant, the team reached the first, difficult step.
Building on earlier published efforts, the team discovered the completed process will need to encompass five stages of specialization from an undifferentiated stem cell to a fully functioning parathyroid-like cell. Each step involves inducing the cell to express the specific genes necessary to guide the process in the desired direction.
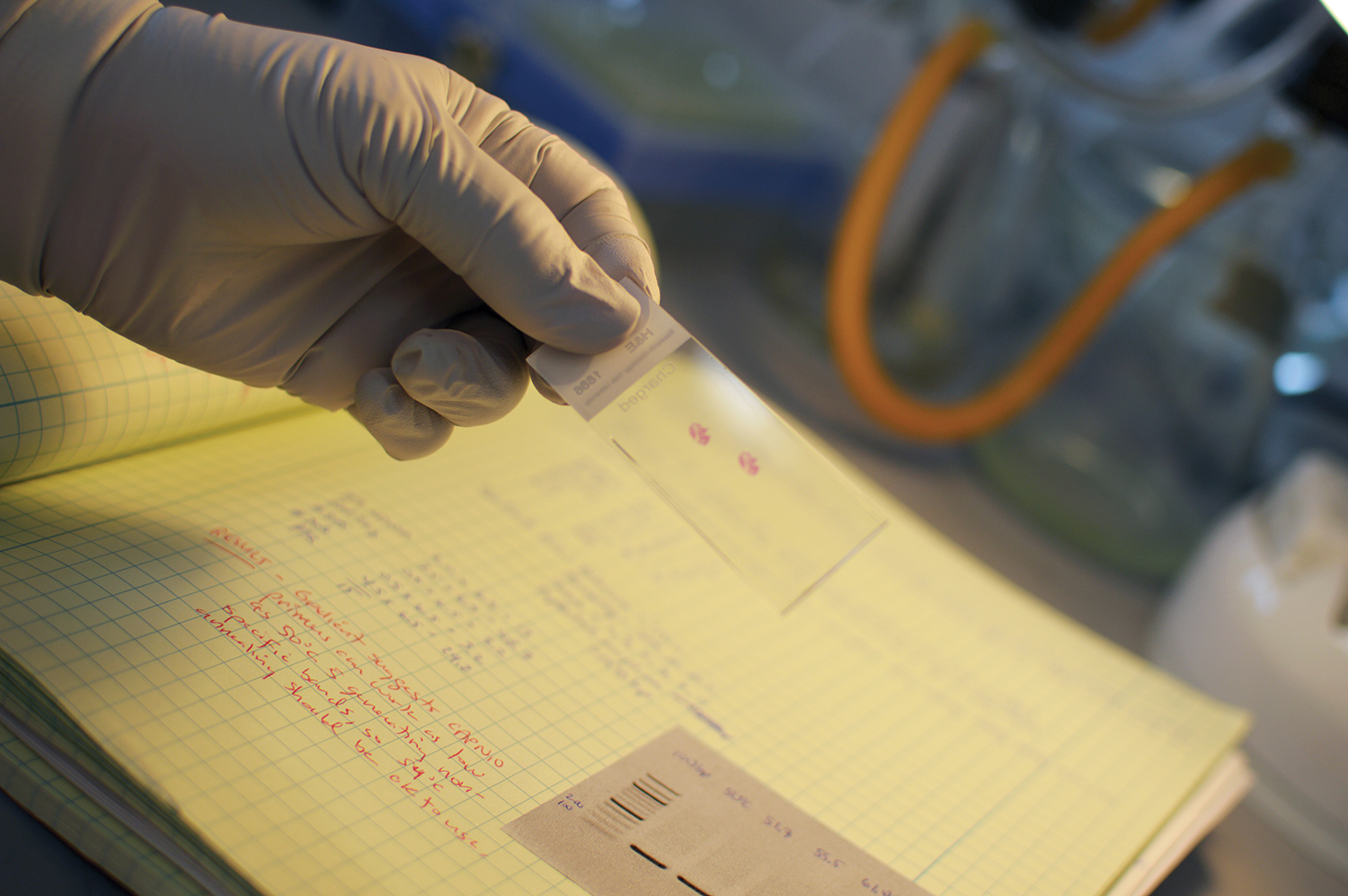
In achieving the first step, the researchers labored 24 hours a day, seven days a week to manipulate chemical stimuli, timing, the growth medium, and temperature to eventually steer stem cells into becoming what is known as anterior definitive endoderm, a type of cell that makes up the inside layer in very early human development and gives rise to internal organs, including parathyroid glands.
“This is intricate, delicate, arduous work,” said Dr. Carolyn M. Mazure, Director of WHRY. “Every step along the way provides benchmarks and creates a model for stem cell researchers to follow in pursuit of treatments for diseases and conditions that diminish human health and well-being.”
With additional funding from WHRY in 2014, Krause began to tackle a separate challenge needed to produce mature parathyroid cells from stem cells: how to test their function by injecting the newly created cells into the body so they attach, survive, and perform the necessary calcium-regulating work of the missing parathyroid glands.
Using an animal model, Krause successfully injected preserved human parathyroid cells into muscle tissue and demonstrated that single cells are a sufficient long-term substitute for the intact three-dimensional architecture of a parathyroid gland. This was an essential step forward, proving that once the stem cell-derived cells are created and purified, they will be able to function upon transplantation.
The Goal: Starting with a Patient’s Own Cells
To date, Krause has worked with stem cells from government-approved banks. But using a patient’s own cells — likely skin cells — will minimize the potential for that person’s immune system to reject the cells. Krause expects these tailored cells, once achieved, to work just as well as the missing parathyroid glands in regulating calcium.
The team continues to make progress toward using a patient’s own cells, walking them back in development so they become what are known as induced pluripotent stem cells (iPSCs), leading them into becoming parathyroid cells, and injecting them back into the patient.
“Our goal is nothing less than personalized regenerative medicine for parathyroid function,” Krause said.
Krause leveraged the findings of the WHRY-funded pilot projects to obtain a pair of larger state grants to advance both arms of this work, teaming with endocrine surgeon Dr. Glenda Callender and genetics and computer science professor Dr. Smita Krishnaswamy, while maintaining her collaboration with Drs. Sosa and Roman.
In January, Krause, who helped establish Yale’s dedicated stem cell center, attended a meeting of 30 researchers from across the country to share notes and reassert their commitment to pursuing stem cell therapy to treat hypoparathyroidism.
“Dr. Krause and Dr. Sosa exemplify the approach to interdisciplinary collaboration and translational research that has been the hallmark of Women’s Health Research at Yale since the beginning,” Mazure said. “These are leaders who embody the endurance and perseverance necessary for intensive research. Even while on opposite sides of the country, they understand the value of sharing expertise, data, and materials to overcome critical health problems that affect women in their daily lives.”
Discovering the Keys to Decode an Unwritten Recipe
So far, no one has successfully proven the ability to use iPSCs to effectively treat a disease in human subjects. The process of growing the cells involves much trial and error, coupled with careful monitoring in the lab — creating something from scratch that the body normally does automatically. Then there is the challenge of getting the cells to survive and function in a patient.
“If we succeed in our work on hypoparathyroidism, it would certainly be relevant to developing other needed therapies,” Krause said. “This is new territory for everyone. Each time we make progress, it becomes clearer what the next steps are.”
In one significant development, Dr. Krishnaswamy conducted a computer analysis to map how the cells within a normal parathyroid gland relate to one another, and she uncovered a diversity of cell types. Some make PTH, others are highly diverse in their makeup and serve different functions entirely, such as providing blood vessels for the gland.
One type is a parathyroid progenitor cell, which is more specialized than a basic stem cell in pushing development toward the target of a mature parathyroid cell that secretes PTH. The data indicate such cells are the ones most likely to attach successfully after injection and may prove to be key to giving a patient long-term parathyroid function.
Recently, the team has successfully tested a method to make stem cells glow red if they “turn on” the gene to make parathyroid hormone. This will allow the researchers to more efficiently produce enough and isolate the right type of cells for implantation.
We didn’t have any data — but we had an important idea to help patients.
Dr. Diane Krause
The latest funding from WHRY, thanks to The Werth Family Foundation, will allow Krause’s team to perform in-depth investigations of normal parathyroid glands to identify the specific composition and function of different compartments within the individual cells.
“Our research is now at a critical point where we need to better understand the basic mechanisms of adult parathyroid gland maintenance and regeneration,” Krause said. “This is the practical knowledge necessary to reach our goal of using these cells to restore normal parathyroid function for patients suffering from hypoparathyroidism.”
Krause thanked WHRY for the center’s longstanding support.
“This work couldn’t be done without WHRY,” she said. “The NIH does not fund science for an idea. They need established concepts, ready to publish. But how do you start?”
Krause recalled her meeting with Sosa and Roman eight years ago.
“We didn’t have any data,” she said. “We had an important idea to help patients and just had to start. For that, we needed a pilot funding source like WHRY for us to take the first steps.”
For more news from Women's Health Research at Yale like WHRY on Facebook, follow WHRY on Twitter, or visit WHRY's website.
For questions, please contact Rick Harrison, Communications Officer at rick.harrison@yale.edu or 203-764-6610.
The Women’s Health Research at Yale Pilot Project Program is supported in part by The Rice Family Foundation, The Werth Family Foundation, The Community Foundation for Greater New Haven, the Maximilian E. and Marion O. Hoffman Foundation, the Seymour L. Lustman Memorial Fund, The Seedlings Foundation, and The Eppley Foundation for Research.