In 2013, actor and director Angelina Jolie underwent a preventive double mastectomy after testing positive for a mutation in the tumor-suppressing BRCA1 gene. That spring, she announced the news in a widely read New York Times opinion piece.
In the op-ed, Jolie discussed how her mother died of cancer at the age of 56 and how the mutation Jolie inherited increased the risks she faced for developing ovarian and breast cancer.
She described the procedures that removed and reconstructed her breasts. And she shared her desire to reassure her children that their mother was doing everything she could to stay with them as long as possible.
She also urged women — particularly those with a family history of breast or ovarian cancer — to seek out professional medical advice and make an informed decision on possible genetic testing and preventive treatment. Mutations on the BRCA1 gene and the similarly tumor-suppressing BRCA2 gene also carry increased lifetime risk for cancers of the pancreas and prostate.
“Cancer is still a word that strikes fear into people’s hearts, producing a deep sense of powerlessness,” Jolie wrote. “But today it is possible to find out through a blood test whether you are highly susceptible to breast and ovarian cancer, and then take action.”
About 12 percent of women in the country will develop breast cancer at some point in their lives. For women with a BRCA2 mutation, that number jumps to 69 percent. A BRCA1 mutation leads to breast cancer in 72 percent of women.
Of note, however, surgical interventions can carry significant known risks in addition to psychological and economic burdens. All without the certainty of clear findings that point toward the wisdom of a particular treatment.
Currently, genetic laboratories can look for well-established disease-causing mutations in specific populations, such as Ashkenazi Jews, who are more likely to pass on any of two clearly defined mutations of the BRCA1 gene or one particular mutation of the BRCA2 gene. People of Ashkenazi Jewish decent with a parent carrying one of these mutations have a 50 percent chance of inheriting the mutated gene from that parent.
However, even five years after Jolie’s announcement, it remains unclear what causes the 95% of total breast cancer cases unrelated to BRCA1/2 mutations.
And not all mutations are alike. In fact, there are thousands of mostly benign variants in BRCA1/2 genes, more accurately called either benign polymorphisms or variants of uncertain significance (or VUS). Some VUS are harmless. Some can be disease-causing mutations. There is no easy way to tell which is which. Treatment decisions following genetic testing classified as a BRCA1 or BRCA2 variant of uncertain significance are based on probabilistic models, not specific risk associated with a patient’s particular variant or variants.
But one of the world’s experts on this subject has been constructing a model to uncover how changes like these in genes lead to disease.
“We’re examining BRCA1 and BRCA2 to understand the progression of cancer at the most fundamental level,” said Dr. Ryan Jensen, Associate Professor of Therapeutic Radiology at Yale Medical School. “We need to recognize what is happening to the genes to create this elevated cancer risk, and then we can better address ways to treat and prevent these diseases.”
Jensen’s work, spurred by a WHRY-funded grant in 2013, continues progress toward a rapid laboratory test that will clear up the ambiguity and help guide patients and doctors toward decisions that can produce the best health outcomes.
“There are thousands of women in the United States with thousands of different alterations to these important genes,” Jensen said. “We need to learn everything we can to help them.”
Uncorrected Errors
In 1990, Dr. Mary-Claire King at the University of California, Berkeley, discovered a gene shared by families susceptible to breast cancer, sparking great interest in biomedical science to link genetics to disease. She called her discovery BRCA1 (breast cancer susceptibility gene 1) for its breast cancer connection. A group of scientists led by Michael Stratton at the University of Cambridge identified the BRCA2 (breast cancer susceptibility gene 2) gene in 1994.
The BRCA1/2 genes work to correct potential tumor-causing mistakes made during the replication of DNA, the material carrying the body’s genetic code that directs the production of proteins and passes traits from parents to offspring. Proteins form the building blocks of cells and trigger biochemical reactions.
But even as people might consider their genetic code to be a permanent part of themselves, DNA is not static. Every time a cell divides, all 3.2 billion base pairs that form a DNA molecule’s coded double-helix structure have to be copied. Sometimes there are mistakes.
“The BRCA1 and 2 genes function like an auto correct function in text messaging,” Jensen said. “When the genes that code for BRCA1 and 2 proteins are mutated and fail to correct DNA damage, genetic mistakes accumulate, eventually leading a cell down a path to becoming cancerous.”
But in order to better understand how these mutations function and what work goes unaccomplished when the gene is not intact, someone first needed to isolate a pure sample of the proteins that the unmutated genes create. This presented a difficult task because of the large size of the proteins, their instability, the complicating presence of other proteins that attach to them, and the low levels at which they can be found in human cells.
In 2010, after six years working in a 4 degree Celsius cold room, Jensen was the lead author on a study culminating a total of 15 years of research and published in the journal Nature to announce the successful purification of the BRCA2 gene’s protein. In 2017, he collaborated with Dr. Patrick Sung, Yale Professor of Molecular Biophysics and Biochemistry, Therapeutic Radiology, and Epidemiology, to successfully purify the BRCA1 protein.
“If that was the hard part, next came the equally hard part,” Jensen said.
So-called truncating mutations in BRCA2, like those found among Ashkenazi Jews, delete an easy-to-spot large section of the protein strand needed to bind to the DNA and are associated with very high cancer risk. If the protein can’t bind to the DNA, it can’t repair the DNA, which leads to the development and spread of cancer.
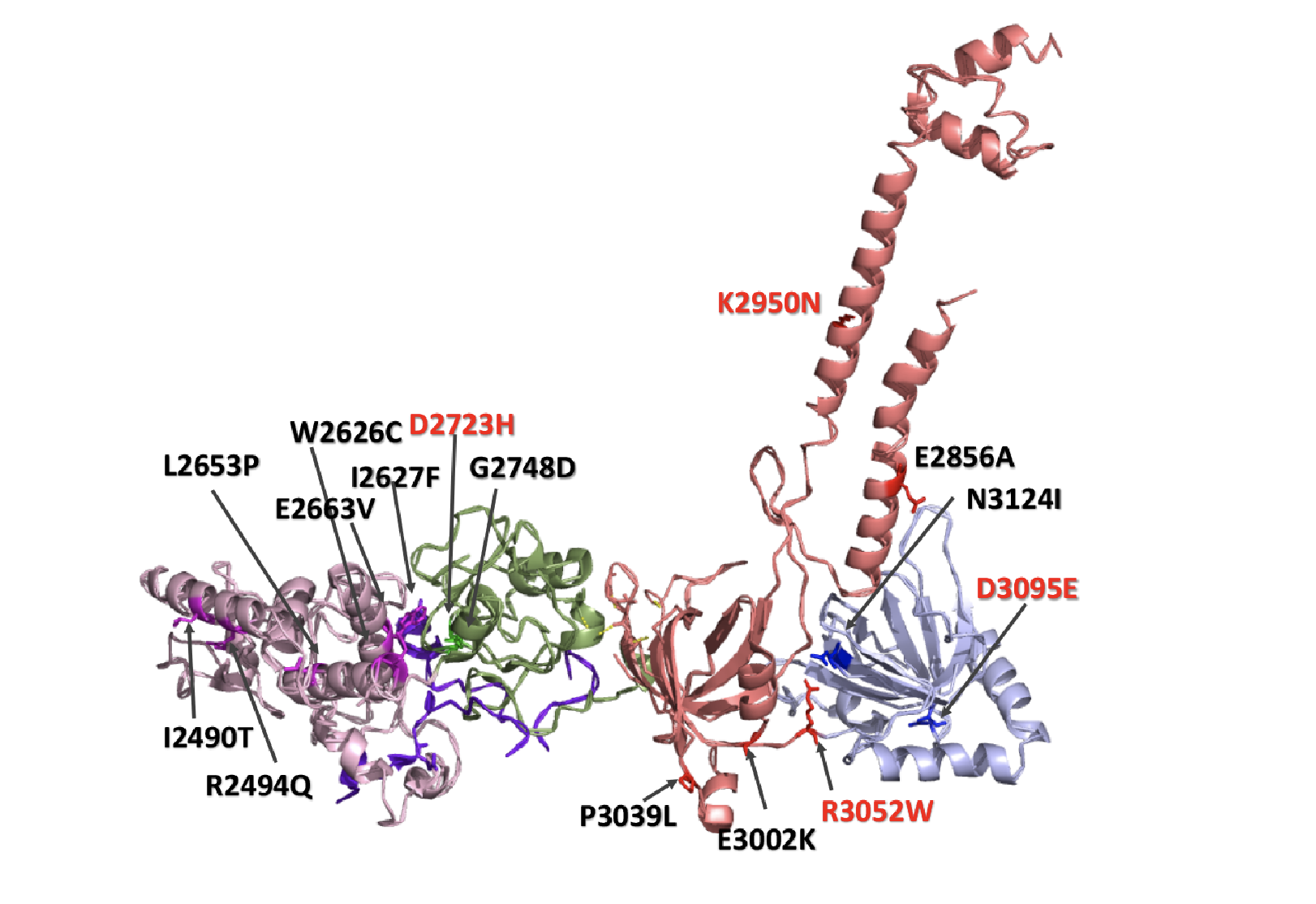
A more subtle variant is called missense, which involves changing a single amino acid, the organic substance that forms proteins. That’s one altered amino acid in a chain of 3,418 amino acids that make up the DNA-correcting protein. Such missense mutations are commonly labeled as variants of uncertain significance because of their relative rareness and difficulty to link to disease.
“How does one amino acid affect a protein and the risk for cancer?” Jensen said. “Answering that question has been keeping us busy.”
Looking Closer
In 2013, Women’s Health Research at Yale funded a two-year study in which Jensen’s team began the painstaking effort of purifying the BRCA2 gene when it contains 10 of the most common variants of uncertain significance and conducting experiments to determine if the alterations in the DNA code affect the function of the intact BRCA2 protein.
“Studying the top 10 can direct us to understand other nearby mutations or similar functions of the protein,” Jensen said. “We are using it as a model to guide us and assess all of these variants that may or may not cause disease.”
Individuals in the general population are not screened for specific mutations. Instead, labs analyze the entirety of their genes to find deviations from a complete set of intact genes assembled by scientists in a database to use as a reference. Such comparisons show a lot of normal variation from individual to individual. These are changes, but not necessarily disease-causing mutations. What Jensen and others are trying to determine is which of the variants are most likely to lead to disease.
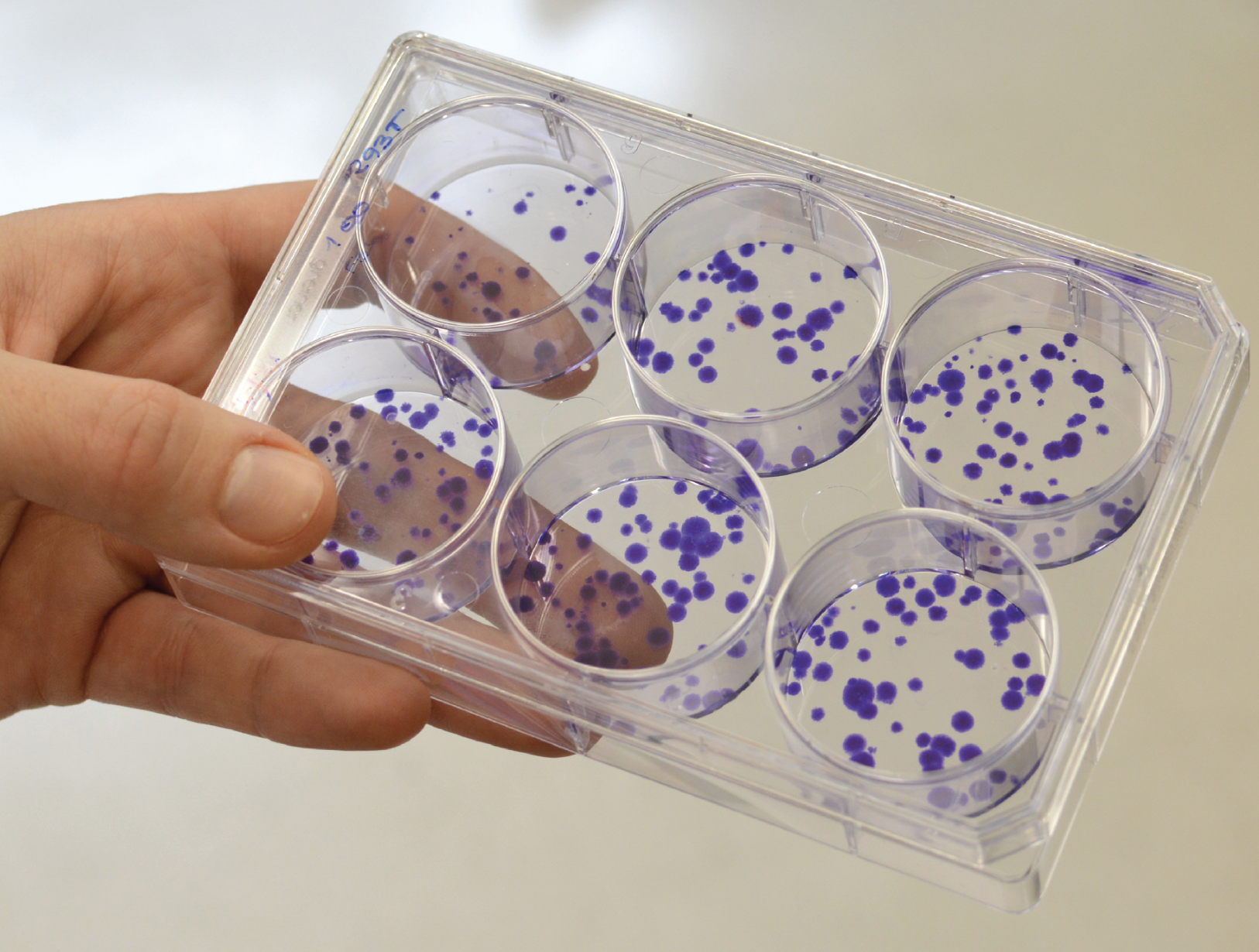
Jensen’s goal is to develop a practical test that can quickly and accurately determine whether an individual’s variant is harmful or not. His WHRY-funded study proved the principle of such a test and its effectiveness in distinguishing harmful from benign BRCA2 variants by comparing those known to be harmful and others known to be harmless as confirmed by studies of patients with the genetic mutations and the presence or absence of cancer diagnoses.
Jensen’s WHRY-funded proof-of-principle study allowed him to successfully apply for a large grant from the National Institutes of Health to continue this work toward determining which BRCA2 variants prove harmful so that patients and their health care providers can make informed decisions about potential treatments.
And the study advanced his lab’s larger goal of establishing a model that can accurately describe and predict the mechanisms that turn a healthy, functioning cell into a tumor that not only survives without an intact BRCA1 or BRCA2 gene, but thrives and spreads.
Toward this end, he will purify more BRCA2 protein samples and examine their structure in crystal form or by using a special electron microscope technique called cryo-electron microscopy (cryoEM) in which samples are cooled to cryogenic temperatures (below -180 degrees Celsius). If successful, he can use these images to create a 3-D picture of the BRCA2 protein to further our understanding of how the protein works and why certain mutations interfere with its normal functions.
“Once we get a handle on what BRCA2 looks like, we can learn so much,” Jensen said. “Where are the mutant amino acids? On the surface? Are they important for interaction with other amino acids or buried inside and not so important? With visual biochemistry we can look at the protein and make predictions.”
Enabling Early Detection and Treatment of Ovarian Cancer
In response to the success of Jensen’s earlier work, WHRY has granted him this year’s Wendy U. and Thomas C. Naratil Pioneer Award to uncover why there is such a high prevalence of ovarian cancer in BRCA2 mutation carriers and offer needed guidance for women to treat or prevent this deadly disease.
About 22,500 women in the country will receive a diagnosis of ovarian cancer this year. And 14,000 will die of the disease. The best chance for survival relies on early detection, but current methods remain inadequate.
“Ovarian cancer is of particular importance for women’s health as it is often diagnosed too late for effective therapeutic intervention,” Jensen said. “By identifying the molecular circuitry disrupted by loss of the tumor-suppressing protein produced by BRCA2, we have the opportunity to expose vulnerabilities that can be selectively targeted or lead to novel biological clues to aid detection and vastly improve the standard of care for this unique population of women.”
In this new study, Jensen will manipulate fallopian tube cells and cells from the surface of ovaries that have been identified as the potential origin of ovarian tumors to determine how the loss of BRCA2 proteins can influence this process.
Jensen has already created fallopian and ovarian surface cells in which he can turn the BRCA2 protein “on” and “off” like a switch. This experimental system will provide a powerful model to test his hypothesis that cells without the BRCA2 protein experience profound genomic instability, a cellular state in which mutations begin to accumulate throughout a person’s genome at an alarming rate.
In the absence of an intact BRCA2 protein, these mutations usually end up killing the cell. But in rare cases and possibly in specific cell types, such as fallopian cells, the cells somehow manage to survive. Jensen’s study is designed to understand at the molecular level how this could happen.
“We have made so much progress in understanding how genes can affect diseases like cancer,” Jensen said, expressing his gratitude for WHRY’s early investment in his work at Yale. “I’m eager and hopeful to see where this work takes us and how many people can benefit from it."
Our 20th Year — WHRY’s Long Fight Against Cancer
In one of WHRY’s earliest breast cancer studies, Dr. Bruce Haffty, currently Chief of Staff at Rutgers Robert Wood Johnson Medical School in New Jersey, demonstrated that BRCA1 and BRCA2 mutations predict a vulnerability to breast cancer recurrence in either the treated breast or the untreated breast.
We need to recognize what is happening to the genes, and then we can better address ways to treat these diseases.
Dr. Ryan Jensen
This landmark study, published in 2002 in The Lancet medical journal, continues to inform clinical decisions about treatments to prevent recurrence.
The Women’s Health Research at Yale Pilot Project Program is supported in part by The Rice Family Foundation, The Werth Family Foundation, The Community Foundation for Greater New Haven, the Maximilian E. and Marion O. Hoffman Foundation, the Seymour L. Lustman Memorial Fund, The Seedlings Foundation, and The Eppley Foundation for Research.
For more news from Women's Health Research at Yale, like WHRY on Facebook, follow WHRY on Twitter, or visit WHRY's website.