April 16 is National Healthcare Decisions Day. The day exists “to inspire, educate and empower the public and health professionals about the importance of advance care planning,” or preparing for future decisions about your medical care if you become seriously ill or unable to communicate your wishes.
In this Q&A, I spoke with Mary E. Tinetti, MD, Gladys Phillips Crofoot Professor of Medicine (Geriatrics) and co-creator of Patient Priorities Care, to discuss aging and how she is reimagining how complex health care decisions are being made. She also shares how she has applied her expertise to help her own parents make health care decisions.
Q: There’s a prevalent stigma against aging in our society. Many people don’t want to think about getting older, let alone prepare for future health care decisions. What can we do to get that attitude to shift?
A: Take any judgment away from being older. Yes, you can highlight the positive parts of aging—the wisdom that comes with it, the feelings of accomplishment, the more adaptable you become—but really, there are good and bad things in every part of life. Aging is just what happens if people have the good fortune of living long enough.
Q: What does National Healthcare Decisions Day mean to you?
A: I believe the day began to make people aware of how important it is to think about advanced care, or what they may want in the future, and identify someone they trust to help them with decision when they’re unable to make them by themselves.
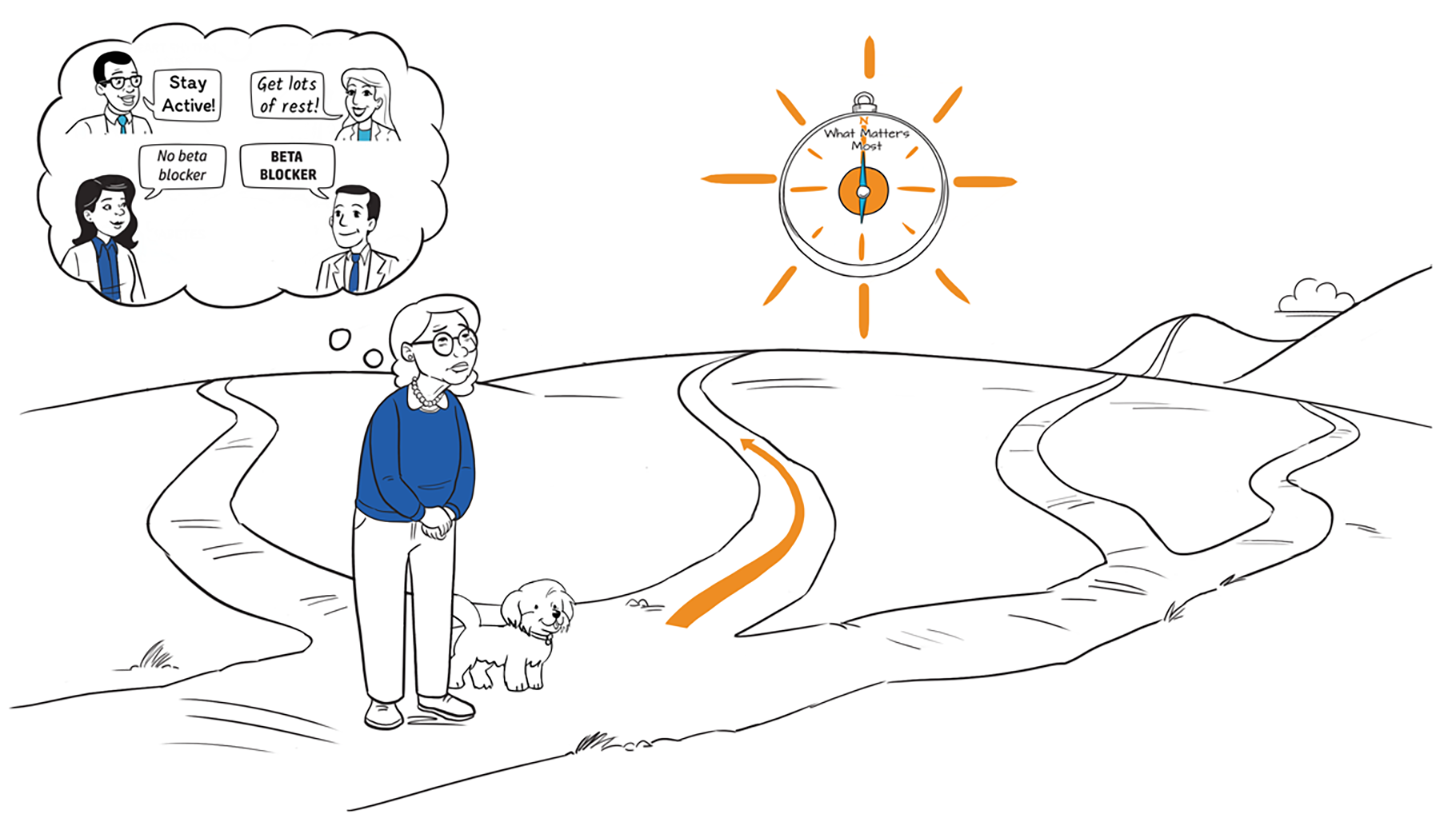
I’d like for people to become increasingly aware of what matters to them today. It’s hard to decide what you’ll want tomorrow because you don’t know what the situation is going to be tomorrow. There's so much more we can do in terms of health care—we’re great at making new advances but not so great at identifying what's most appropriate for individual people. That can only happen if people are aware of what matters most to them because there will always be tradeoffs, which happens when someone needs to balance the benefits and burdens of care or choice between the outcomes they value most. I would like to see National Healthcare Decisions Day focus as much on today as tomorrow.
Q: You’re the co-creator of Patient Priorities Care, an approach to care that helps patients and care partners focus decision-making on what matters most: patients’ own health priorities. Where did the idea for Patient Priorities Care come from?
A: Through my observations from taking care of older adults with multiple chronic conditions and complex life stories for decades, it became clear that the way we make decisions about each condition in isolation and focus on them independently didn't make a lot of sense. It worsens the complexity for patients and health professionals rather than simplifying—managing each condition separately puts burdens on people from treatments that may not be very beneficial. It seemed like there was a better way.
Around the same time, the area of multiple chronic conditions was emerging. So much of research up until probably the 2000s was disease-focused, even in geriatrics. Amy Berman from The John A. Hartford Foundation approached me to ask if I would lead efforts to focus on primary and specialty care as it related to older adults. Patient Priorities Care was built on the idea that disease by disease guideline-based care may not be best for people who have multiple chronic conditions. Emergent work from researchers like my colleague, Terri Fried, MD, Humana Foundation Professor of Medicine (Geriatrics), who found that older adults with severe and advanced conditions varied in what they wanted from their health care, also formed the foundation. Everybody didn't want the same thing.
It became clear that the way we make decisions about each condition in isolation and focus on them independently didn't make a lot of sense. It worsens the complexity.
Mary Tinetti
I thought, “Okay, if we're not sure whether there's one right answer or whether disease-based care alone worked and there were a lot of other things besides diseases that were getting in the way of what mattered to people and people varied in what mattered to them, then what is the logical solution?”
Ask people what matters to them about their health and make your decisions based on it. That was the evolution of Patient Priorities Care. Dozens of people weighed in on it. That’s it at its core; that's how it came to be. That was in about 2013.
Q: Have you personally noticed family members, friends, or anyone in your life struggle with making health care decisions?
A: Yes, with both of my parents. My mother had multiple conditions and was getting frail. She had bad heart failure, severe spinal stenosis—back pain that made it difficult for her to get around—and she was having more and more hospitalizations and was less able to do the things she wanted to do. My father was providing more and more care.
It was about six o’clock one morning in I believe 2004. I had gone to Flint, Mich. to visit with her in the hospital. I was planning to fly out, and I found her lying in bed short of breath. It was clear that her heart failure was worse, so that was easy to treat— the doctor ordered more Lasix, and she was better. But then she said to me, “Honey, I don't ever want to come back to the hospital again.” She was clear that what mattered most to her was for the time she had left, she wanted to be home. So, we were able to make that happen for three years with wonderful help from home hospice, her primary doctor, and most importantly, my father.
With my father, it was a little more difficult. He was actually very healthy; he took care of my mother wonderfully. In fact, he died last July at the age of 100. He was less clear about what he wanted. He knew he didn't want to go to the hospital, and he really didn't want to get a lot of health care. But he wasn't quite sure what he was willing to do for some of his pain and other issues. Despite that, I was still able to walk him through the health priorities identification process, and he never went to the hospital again either. To me, it’s a success story—neither of them spent any of their last years in the hospital.
Q: Why is it important for patients with multiple chronic conditions to be empowered in their health care decisions?
A: Most people who get to age 65 or 70 and many people younger than that, are going to have multiple chronic conditions. They may be living it, but they really haven't thought about the implications that has.
You're the expert in what matters most to you, and your clinicians are the experts in how to help you get there. We all want to live as long as possible, to not have to work at it, to be completely functional and have no discomfort. That doesn't happen. There are tradeoffs, and only you can know what matters most to you in the face of those tradeoffs. If people are unaware of what they want and what they’re willing to do, they're going to get care they don’t want.
Especially as health care has gotten more fragmented and you're going to more and more clinicians, you don't know whether you'll be seeing the same person every time. it’s even more important that each person is responsible for and communicates their own priorities. It improves your relationship with clinicians, too. Some people think their clinician knows what matters to them, so they wonder why they should have to tell them. While they may know a lot about you, they don't know what matters most to you in the face of a tradeoff. The more they know, the more they can help you make the right decision for you.
Q: How you would recommend a patient bring up Patient Priorities Care to their health care team?
A: If they have access to a computer, go to MyHealthPriorities.org. It's a systematic way to help you identify what matters most to you about your health and your health care, and at the end of it, there are some tips on how to communicate that with your clinician. If you don’t like to do things on the computer, there's also a printable version.
The more specific you are about what you want, the easier it is for your clinicians to use that information and make decisions with you. Don't be afraid about bringing it up because clinicians do care about what you have to say.
Patient Priorities Care (PPC) offers evidence-based tools and resources to help patients, care partners, and clinicians focus decision-making and health care on what Matters Most: patients’ own health priorities. Patient Priorities Care is suitable for any patient, but especially older adults managing multiple chronic conditions. PPC is a Yale research project from the Department of Internal Medicine’s Section of Geriatrics, led by co-creator Mary Tinetti, MD, who is the principal investigator on the research grant. PPC is now focusing efforts on spreading awareness and training clinicians across the U.S.