The coronavirus has upended the healthcare sector. What follows are five viewpoints from fellows in the section of Cardiovascular Medicine. Each demonstrates how a crisis can provide a window for innovation creativity. Navigating the coronavirus explores how our community is adapting during the pandemic.
Sumeet Pawar, MD:
The son of Indian physicians, Sumeet Pawar, MD, was familiar with the constraints of caring for patients in a resource-limited setting. Pawar studies how digital technology improves quality and increases access to care. Now a third-year fellow in the section of Cardiovascular Medicine, Pawar chairs the Yale Resident Fellow Senate Quality Improvement Council.
Electronic consultations or eConsults have been available for a decade. Many medical providers lacked the momentum to implement this service until now. Cardiology eConsults enable physicians to identify a health concern before it escalates.
“The first question is often how will this affect patient care,” said Pawar. eConsults act as a filter, allowing physicians to review medical health records and important data. The benefits include alerting physicians to high-risk patients who may have missed an appointment or forgot to refill a prescription. Studies also show that patients save money when compared with traditional face-to-face visits. Pawar has been developing an eConsults process with Daniel Price, MD. Educating primary care providers about the cardiology e-consult process is a crucial first step to scaling-up this process data in the Journal of Telemedicine and Telehealth suggests.
Elliott Miller, MD: 
As the ICU fills with COVID-19 patients, cardiology fellows are volunteering to work in the ICU. Third-year clinical fellow Elliott Miller, MD was one of the first. He recently completed a week-long rotation as a COVID-19 ward attending. Miller has prior training in critical care with the National Institutes of Health. He wrote a tip sheet to help treat COVID-19 patients with acute respiratory distress syndrome (ARDS).
Yale New Haven Hospital has multiple units to treat patients in critical condition. Under the direction of Joseph Brennan, MD, the Coronary Intensive Care Unit has evolved in recent years. “As health care systems respond to the coronavirus, the gaps that exist between these two units are blending,” Miller said. In the future, we could see this trend become the norm. Miller outlined potential training pathways to care for a diverse ICU population in Cardiac Critical Care: Training Pathways and Transition to Early Career.
Natalija Odanovic, MD:
As a result of the coronavirus, fellows provide overnight and weekend care for cardiovascular inpatients and consults. Second-year fellow clinical fellow, Natalija Odanovic, MD, has been working with two other senior fellows Sam Reinhardt, MD, and Attila Feher, MD, on this transition. Together they organize a biweekly EKG conference where Lynda Rosenfeld, MD, shares challenging cases that the fellows review and discuss together.
Jennifer Kwan, MD, PhD: 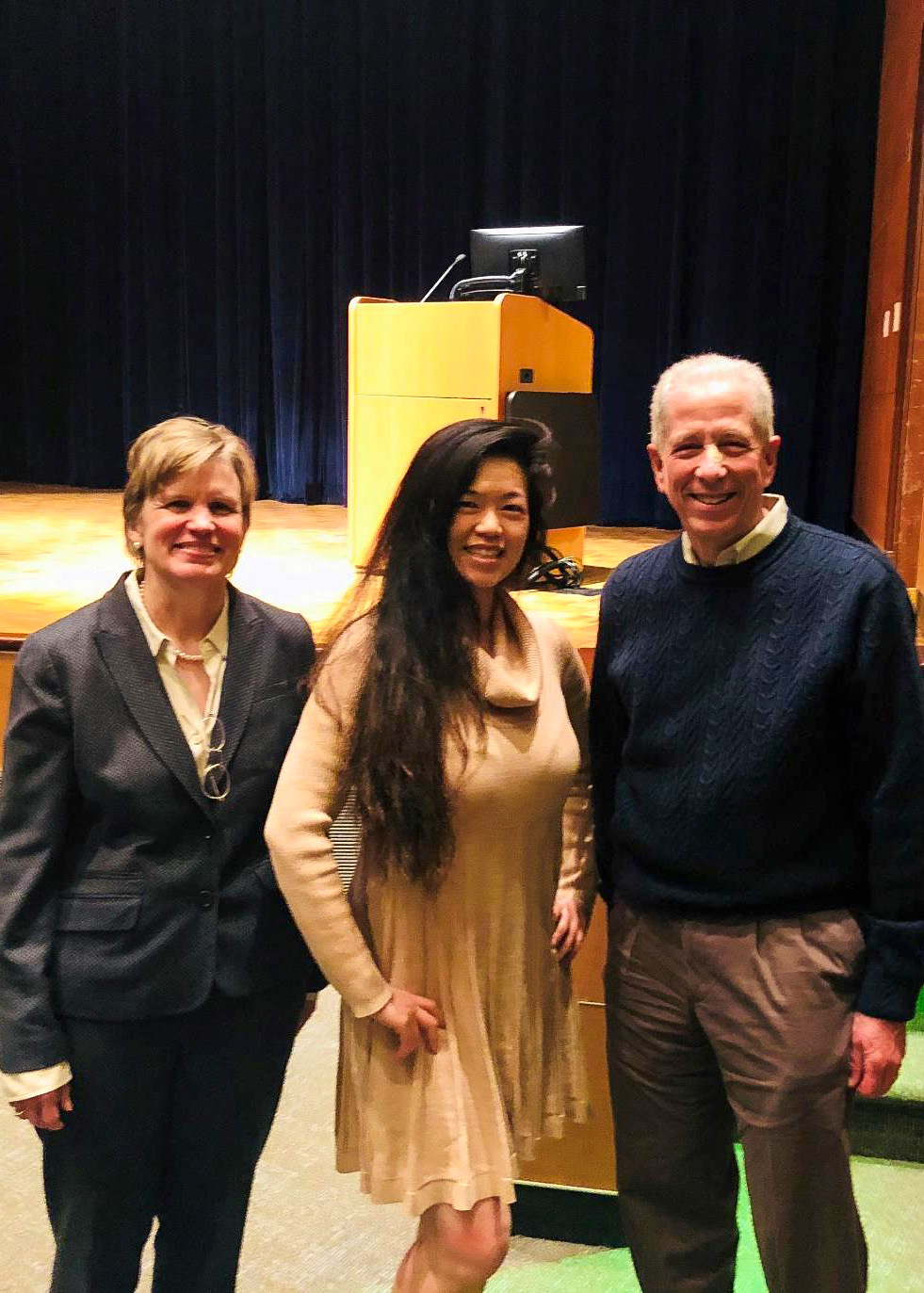
The coronavirus has disrupted both research and clinical training. Jennifer Kwan, MD, PhD, a second-year clinical fellow, has been leading efforts to understand how the pandemic impacts physician-scientists (PS). Under these new circumstances, some face job uncertainty while others are eager to combat the coronavirus.
Kwan surveyed PS to understand how the coronavirus impacts researchers. PS account for 1.5% of the U.S. physician workforce, Kwan wrote in a recent article she co-authored with Evan Noch MD, PhD. The article discusses the APSA’s Early Career Physician Scientists initiative to build a diverse pipeline of academic medical faculty. The article also includes an interview with Robert Alpern, MD, the former dean at the Yale School of Medicine.
This process has brought the mentors, fellows, and attendings even closer. People are finding innovative ways to provide the best cardiovascular care in difficult circumstances.
Kerrilynn Carney Hennessey, MD
The results of the survey were shared during a webinar Kwan co-hosted on behalf of the APSA earlier this month, How to Support and Retain Early Career Physician-Scientists & Response/Insights on the Impact of COVID19 on this cohort. The speakers included Sindy Escobar-Alvarez, PhD, from the Doris Duke Charitable Foundation, Dean Nancy Brown, MD, and NIH Director, Francis S. Collins, MD, PhD. Her manuscript assessing a nationwide cohort of MD PhD and MD trainees and their career intentions for academic and research careers was recently published.
Many prominent physician scientists have noted that, “I don't think we can see our way through this pandemic without physician scientists." Kwan is part of a research team that includes the interim chief of Hematology at Yale Cancer Center, Stephanie Halene MD, PhD, and two cardiovascular medicine faculty Arya Mani, MD, and John Hwa, MD PhD. The researchers hope to understand the molecular mechanisms and differences between critically ill COVID-19 patients and those who have mild cases. Particularly, patients who develop adverse cardiac outcomes such as heart failure or myocarditis. Kwan and the researchers are evaluating factors such as patient genetics/epigenetics and characterizing immune cell, platelet profiles and function. Kwan has also been collaborating with residents, recruiting and reviewing COVID-19 patients, and sending samples for sequencing and molecular analyses. Halene and her lab have been preparing samples around the clock to enable this research.
Kerrilynn Carney Hennessey, MD: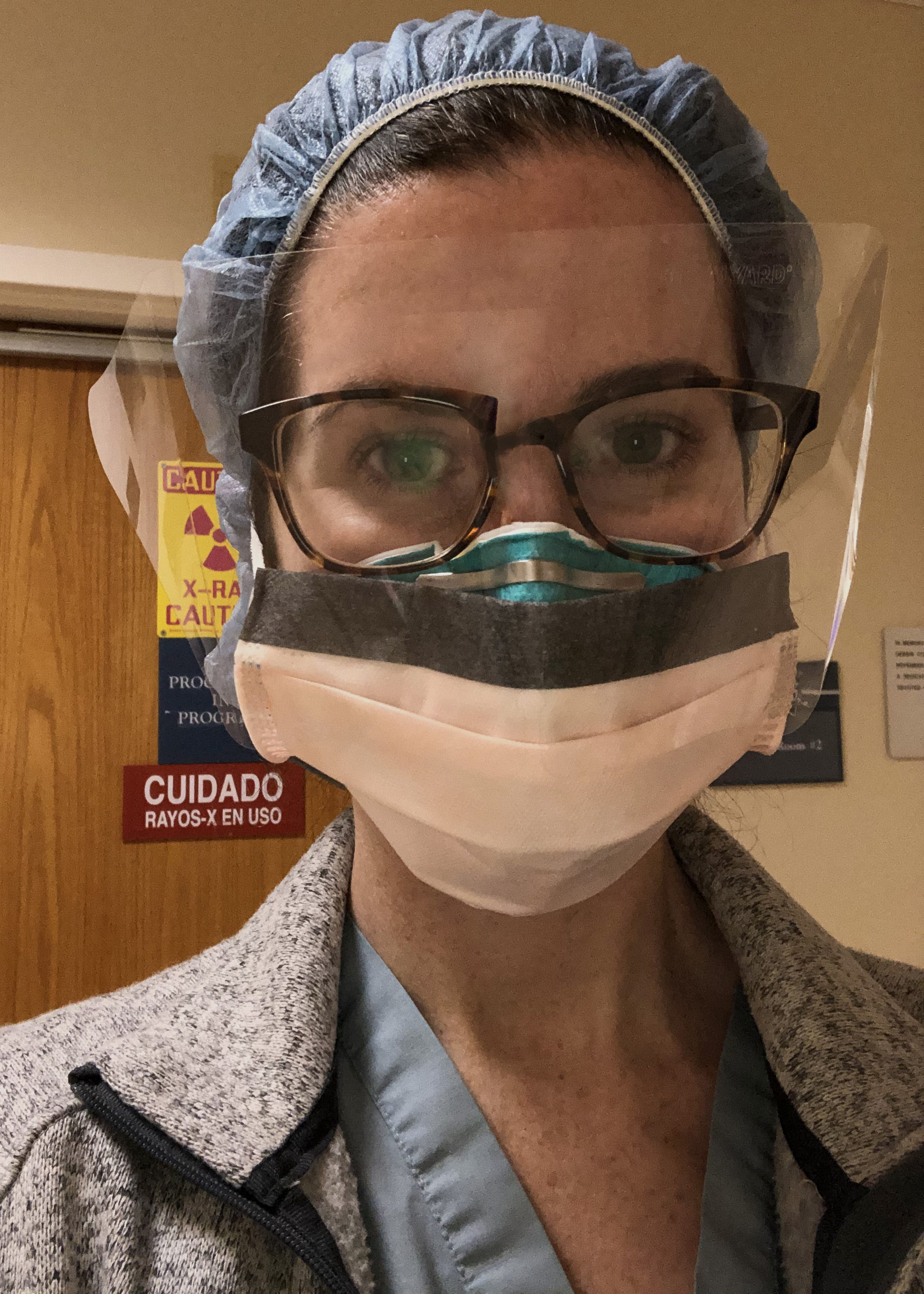
Grappling with resource utilization is new for many physicians in the U.S. If a patient is under investigation for COVID-19, hospitals must determine when to defer medical procedures without running the risk of underserving patients or putting lives at risk. Since March 19, third-year clinical fellow Kerrilynn Carney Hennessey, MD, has led these efforts in the echo lab. Carney Hennessey developed a system to triage echocardiography requests during COVID-19 with echo lab director, Lissa Sugeng, MD, Robert McNamara, MD, Kamil Faridi, MD, Vratika Agarwal, MD, and cardiovascular imaging fellow Aaron Soufer, MD. Carney Hennessey and a team of cardiology fellows analyze echocardiography requests for patients with possible (test pending) or confirmed (test positive) COVID-19 to determine the urgency of the exam. The overall aim of the triage process is to perform echocardiograms that are needed for urgent clinical decision-making while reducing the number of providers exposed to COVID-19. Carney Hennessey and her team reviews the patients’ medical chart before calling to evaluate the urgency of the procedure and coming to a shared decision about whether the echocardiogram can wait. All of the interactions are documented. Members can track decision making and keep the lines of communication open with both the primary team for inpatients and primary care providers for outpatients.
A cardiac imaging fellow or a general cardiology fellow has been assigned to perform this role 24/7 since March 19. In the past few weeks, this triage process has screened over 50 patients who were either positive or under investigation for COVID-19. Half of that group eventually tested positive. Ultimately, the team decided to perform the test on nine patients. “It’s been difficult to navigate,” she said. “Because the situation is so fluid and the volume of patients is expected to increase.” The uncertainty requires vigilant monitoring from the fellows and the clinical staff.
The team collects data on this initiative for safety and efficacy, “It’s been educational on the whole,” she added. The time that Carney Hennessey spends away from the hospital is devoted to monitoring data and creating tools and resources to implement these strategies in other departments. “This process has brought the mentors, fellows, and attendings even closer. People are finding innovative ways to provide the best cardiovascular care in difficult circumstances,” she said. For Carney Hennessey and her team, the coronavirus has been an opportunity to pause and reexamine patterns of resource use. “There is a difference between wanting information and needing information,” she added. Even routine tests and procedures have to be closely monitored to balance the risk-benefit ratio.
For the latest information about Yale’s research and clinical efforts to combat COVID-19, please visit covid.yale.edu.